Review Ditsapelo M. McFarland's presentation on cervical cancer.
by Ditsapelo M. McFarland
Several years ago I registered for a course at UMass University, Amherst, entitled “Epidemiology of Cancer.” During a literature search, I realized that cervical cancer was a major problem for women worldwide, specifically in developing countries. I had no idea about the situation of cervical cancer in Botswana. Upon entering Boston College for my doctorate, I decided to intensely study cervical cancer for my dissertation. I have since written several articles on cervical cancer and screening in Botswana. My purpose in this article is to share the findings of the recent study entitled, “Associations of demographic variables and the Health Belief Model constructs with Pap smear screening among urban women in Botswana” (McFarland, 2013).
Introduction
Cervical cancer is the most common cancer and the leading cause of cancer deaths among women in Botswana and the incidence is steadily rising. It is estimated that every year, 163 women are diagnosed with cervical cancer and 83 die from the disease. Projections further indicate that by 2025 there will be 224 new cases of cervical cancer and 122 deaths from the disease (WHO, 2010). The high mortality from cervical cancer may be related to late presentation at health facilities. Evidence from developed countries indicates that cervical cancer is preventable with regular cervical cytology screening using Pap smear. Pap smear has the ability to detect minor cervical changes early when they can be treated and before they can progress to the invasive stage of the disease. Despite the availability of the screening services that are offered free of charge in most urban Government clinics in Botswana, most women in such areas do not screen regularly for cervical cancer. Pap smear services are used largely for gynecological problems or as part of other services, such as family planning and maternal and child health, rather than for preventive purposes (Botswana National Cancer Registry, 2007). An earlier study (McFarland, 2003) reported inadequate or lack of information about cervical cancer and screening as a major barrier to screening, particularly among women with lower socioeconomic status. In developed countries, factors such as age, income, ethnicity, personal and cultural beliefs, have been identified as influencing the uptake of cervical screening in such countries (Harlan, et al, 1991). Such factors have not yet been fully explored in Botswana, hence this study.
The Conceptual Framework
The study was guided by the Health Belief Model (HBM). The HBM was developed in the 1950s to explore reasons for low participation in preventive programs that were offered free of charge The model purports that an individual’s decision to take a preventive measure against a particular disease, such as cervical cancer, is influenced by four beliefs:
(1) Perceived susceptibility to that particular disease (2) Perceived severity of the disease in question if contracted and left untreated, (3) Perceived benefits of the preventive measure such as the Pap smear test, and (4) Perceived barriers to a preventive action, such as embarrassment associated with the test. Furthermore, cues or stimuli such as fear of the disease or illness symptoms (internal cues) and publicity or educational material (external cues) are needed to trigger appropriate action (Rosenstock, 1974).
Sample and methods
The study included a convenience sample of 353 asymptomatic women aged 30 years and older who were living in Gaborone, the capital of Botswana. Only black women of African descent were included in the study to avoid the influence of foreign belief systems. Because of the nature of the study, the sample selection was also limited to women who were able to complete an English questionnaire and who knew about the Pap smear test and had no history of hysterectomy (surgical removal of the womb) or cervical cancer. Data were collected using a demographic questionnaire and items of the Health Belief Model measured on a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). Data analysis included descriptive statistics for demographic variables and bivariate and ordinal (logit) regression analysis to determine the associations of demographic variables and the Health Belief Model constructs with having had a Pap smear.
Results
Demographic variables
Ninety percent of the participants were between 30 and 49 years of age, with just under half (46%) married and more than three-quarters (77%) having greater than secondary education. The vast majority were employed (92%) and in the service delivery sector (42%). Just more than three-quarters had health care insurance (76%), and 69% had a regular health care provider, with the majority (69%) having a physician as their regular health care provider.
Pap smear practices
Just over three-quarters (77%) of the respondents had ever had a Pap smear, with half (50%) of those having asked for this test to be included in their regular checkups. Two thirds (67%) had their Pap smear at a private doctor’s office, with 62% having heard about it from their health care providers. The rest of the participants (33%) had a Pap smear either at a clinic or a hospital. Just more than half of the participants (52%) had one to two Pap smears in the last 5 years. Only 18% had the recommended four or five Pap smears during the last 5 years. Major barriers for women who had ever had a Pap smear included “laziness” and Pap smear not seen as important. Women who had never had a Pap smear cited limited information about Pap smear screening and financial constraints as their major barriers.
Associations of demographic variables with ever or never had Pap smear
Only two variables were significant predictors of whether or not a participant had ever had a Pap smear: having health care insurance (P # 0.0005) and having a health care provider (P # 0.0005). Women with health insurance were more likely than those without health insurance to have had a Pap smear test (91% vs 36%). Similarly, women who had a regular health care provider were more likely than those without a regular health care provider to have ever screened for cancer of the cervix (94% vs 42%).
Associations of the Health Belief Model components with ever or never had a Pap smear.
Women strongly perceived the benefits of getting Pap smears and the severity of cervical cancer. However, there was no significant relationship between Pap smear screening and Health Belief Mode constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. Women who had ever had a Pap smear and women who had never had a Pap smear were very similar with respect to beliefs of the Health Belief Model. The Profiles of responses for both groups were very similar. This information is displayed in Figure 1.
Figure 1: Box Plot of Association of Smear use with the Health Belief Model Variables (n= 353)
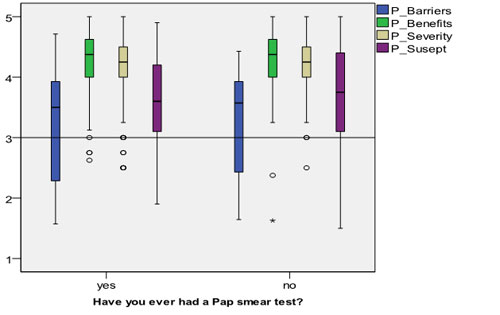
Note: The circles shown in the graph represent outliers and the star represents an extreme value.
Discussion and Conclusion
These findings are consistent with those of an earlier study by McFarland (2003). In that study, the majority of the women had medical insurance and received their Pap smears from private practitioners, who reportedly informed them about the importance of early detection. However, only a few of the respondents (18%) had regular Pap smear tests. Similarly, these women with access to sources of information cited “laziness” as their major barrier to regular Pap smear screening. The author concludes that women in this study are informed about cancer of the cervix and have access to screening. However, attitudes toward screening play a major role as barriers to screening for women who had ever screened. These attitudes were evidenced by the women reporting “laziness” as a major reason why they did not screen regularly. In light of the high incidence of HIV/AIDS in Botswana, these attitudes toward Pap smear use could significantly contribute to an increase in the incidence of cervical cancer, and they suggest a need to be further explored. Unlike in developed countries where cervical cancer is diagnosed at a later age, in developing countries including Botswana, women as young as 15 years of age are diagnosed with cervical cancer, which further indicates the need for services that can be available and accessible to women of all ages and localities.
References:
Botswana National Cancer Registry (2007) Analysis of Registered Cancer Patients 1986–2006. Department of Public Health Disease Control Unit: Gaborone, Botswana
Harlan, LC., Bernstein, AB., & Kessler, LG (1991). Cervical cancer screening: Who is screened and why?. American Journal of Public Health, 81(7); 885-890.
McFarland, D. (2013). Associations of demographic variables and the Health Belief Model constructs with Pap smear screening among urban women in Botswana.” International Journal of Women’s Health, 2013:5 709–716
McFarland DM. Cervical cancer and Pap smear screening in Botswana: knowledge and perceptions. Int Nurs Rev. 2003; 50(3):167–175.
Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;24:238–335.
World Health Organization/Institut Català d’Oncologia. (September 15, 2010). Human papillomavirus and related cancers in Botswana. A summary report Update. Available from: http://www.hpvcentre.net/statistics/reports/BWA.pdf. Accessed May 14, 2013.
Youtube video: http://dvpr.es/158pcaY
For further information, please contact:
Todd Wilson
Strategic Communications Director
p – 516.237.8634
e – twilson@adelphi.edu
